January 11th, 2019 was seeming to be a typical Pacific northwest winter morning. A cool rain was gently falling on the lofty Douglas firs and burly cedars, dripping down to the forest floor below, where physician associate Mike Jones was hiking with his Saint Bernard, Greta—boots and paws leaving their mark in the black humus between the sea of bracken ferns. Mike had taken a day off from managing his busy headache treatment clinic, to train for a month-long trek across Greenland in the coming summer. Before that day was over, Mike would find himself in an ICU, his attending physician at his bedside warning, “Mr. Jones, you need to call your children home. We are doing everything we can to save your life but what we are doing isn’t working. Your potassium is still almost nine.”
By the time of discharge from the hospital two weeks later, through the insight offered by copious blood tests and kidney and bone marrow biopsies, he had a diagnosis of Multiple Myeloma with associated renal failure. He started hemodialysis for 16 hours per week and an aggressive induction chemotherapy program to prepare for a stem cell transplant, his 38-year career as a PA abruptly ending, never to see the interior of his office, his colleagues, or his patients again.
The stem cell transplant required Mike to go on a protective quarantine, typically lasting six months but was extended for two more years due to the COVID pandemic. It was the perfect melancholic storm. Losing his career, friends, health, and future, and living alone as a hermit on a mountain lake. His wife, a hospital administrator, working long hard hours due to the same pandemic.
For over thirty years, Mike had a hobby of writing, having authored over thirty articles for medical journals and eight books. He decided, for his own mental health’s sake, that he needed to write again, this time an epic novel, a much higher level of writing than anything he had attempted before. As a gift to his profession—which had served him so well—he knew a physician associate would be the protagonist in the story, who would showcase to the world what advanced practice clinicians can do. To engage readers, the story had to be enthralling and well written. Mike employed some of the best editors in the business to look over his shoulder as he wrote, guiding his words to be their best.
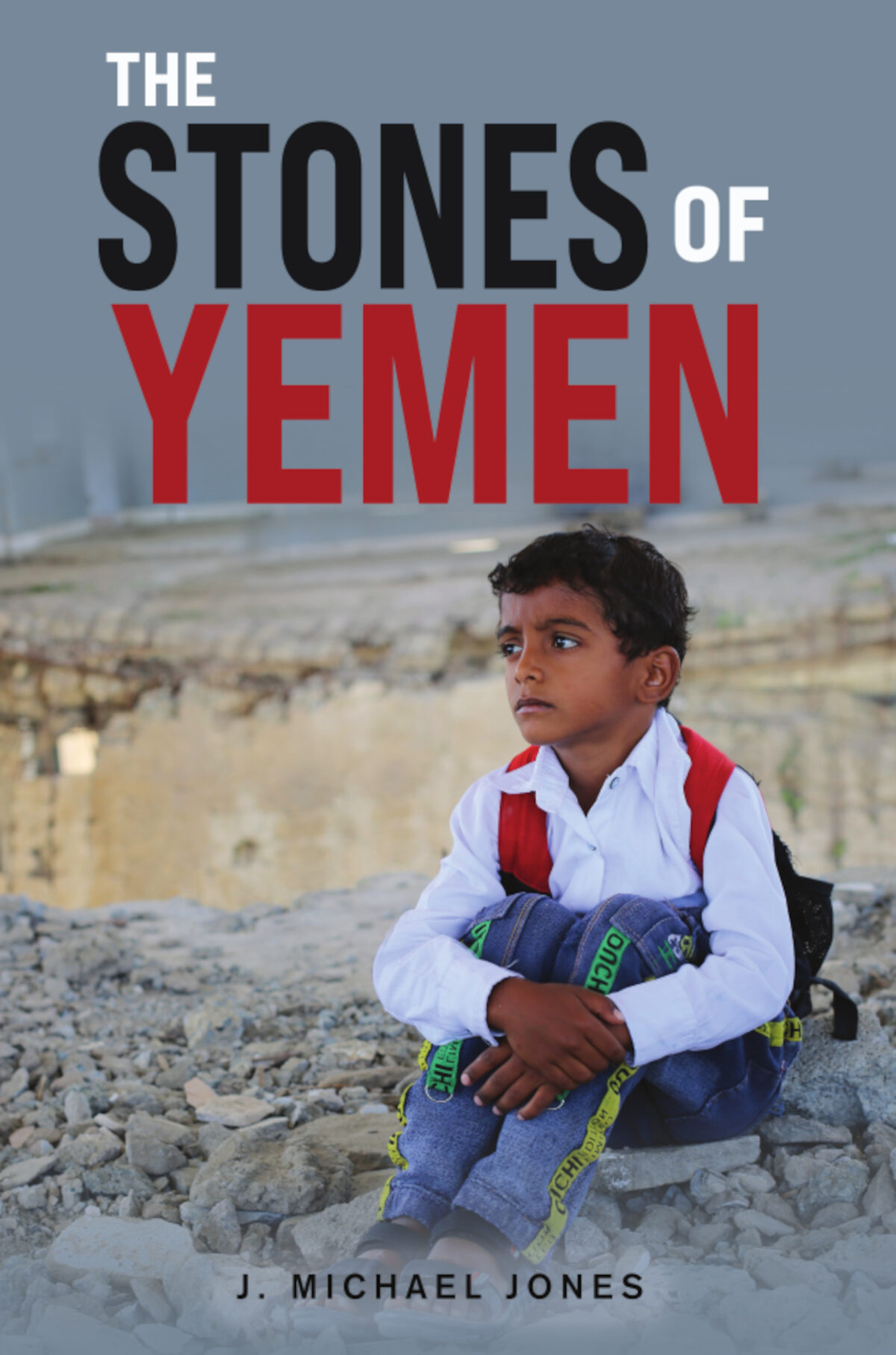
The resulting book, The Stones of Yemen, is a thinking man / woman’s thriller and it is about bereavement. But it is also about sailing, romantic love, political hate, retribution, forgiveness, and hope told on the backdrop of Yemen’s brutal civil war. When they released it in February, it quickly became the best-selling PA book and all the reviews have been glowing. The print copies are available through all bookstores, the eBook format is available for free to Kindle Unlimited subscribers or to purchase on Amazon. An audiobook format is available exclusively at BookBaby Shop .
*Stay tuned Part 2 coming soon!
 J. Michael Jones started writing in the early 1980s, publishing over thirty articles in national medical journals, and The Stones of Yemen is his eighth book, five of them fiction. He had a thirty-eight-year career as a physician associate and worked in refugee camps in Pakistan, Afghanistan, Cyprus, Oman, UAE, Egypt, and Nepal. In addition, he hosted twenty Yemeni students over two years in the U.S. Besides his medical studies, he has a degree in Arabic from the American University in Cairo, which was invaluable during the research for this book. Michael resides with his wife Denise in Washington’s San Juan Islands, where he writes full time. They are the parents of five grown children and one hairy Saint Bernard.
J. Michael Jones started writing in the early 1980s, publishing over thirty articles in national medical journals, and The Stones of Yemen is his eighth book, five of them fiction. He had a thirty-eight-year career as a physician associate and worked in refugee camps in Pakistan, Afghanistan, Cyprus, Oman, UAE, Egypt, and Nepal. In addition, he hosted twenty Yemeni students over two years in the U.S. Besides his medical studies, he has a degree in Arabic from the American University in Cairo, which was invaluable during the research for this book. Michael resides with his wife Denise in Washington’s San Juan Islands, where he writes full time. They are the parents of five grown children and one hairy Saint Bernard.
Disclaimer: The viewpoint expressed in this article is the opinion of the author and is not necessarily the viewpoint of the owners or employees at Healthcare Staffing Innovations, LLC.