physician assistants
Tag89% of Patients Consult “Dr. Google” First
Dr. Google is in. 89% of patients queue up Google and search for their symptoms before going to see a medical provider. But this isn’t exactly a good thing.
PAs to Prescribe Medical Marijuana in NH
New Hampshire’s Governor signed a bill on Friday, expanding the list of providers who are allowed to prescribe medical marijuana to include physician assistants.
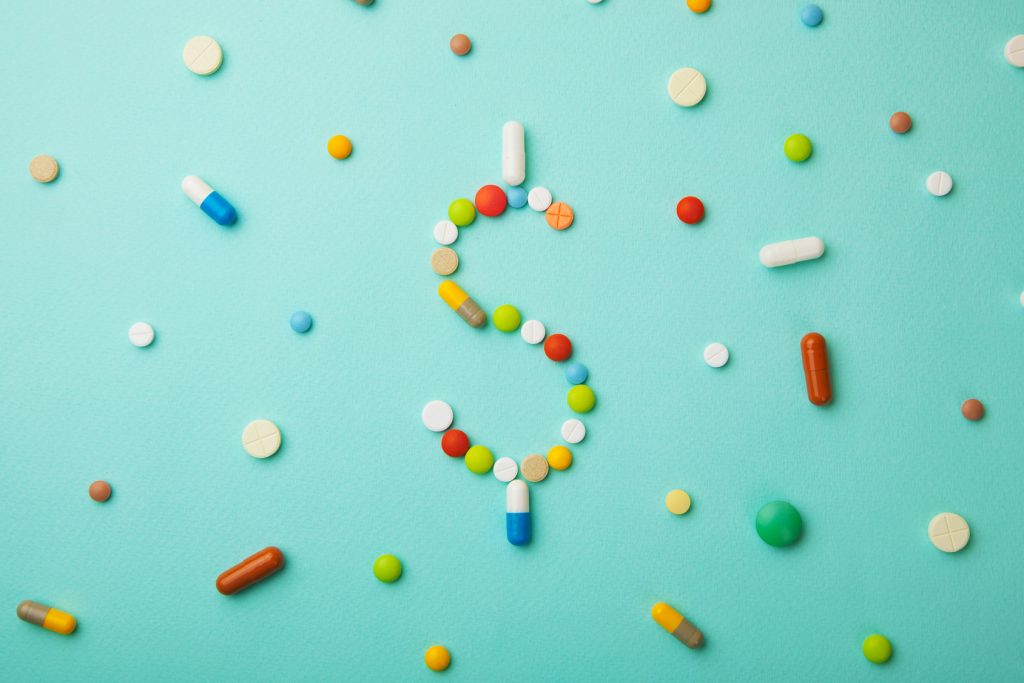
How Much PAs and NPs Make in Every State
How much do PAs and NPs make across the U.S.? We found out. How does your salary stack up against the average?
Maine Law Allows PAs, NPs, Midwives to Perform Abortions
When the bill goes into effect next June, Maine will be the eighth state to permit advanced practitioners to provide abortion services.
VA Study Supports Advanced Practitioner Led Care
A new study has found no clinically important differences in patient outcomes, regardless of whether their provider is a physician, PA, or NP.
Report: PAs/NPs Provide Similar or Better Care than Doctors
A new report from a World Health Organization team indicates that non-physicians, such as PAs and NPs, provide comparable care to that of physicians.
Rebranding of PA Title Moves Forward
The AAPA has announced they have selected a world-renowned branding firm to begin investigating rebranding the physician assistant title.
APRNs and PAs Ranked Among Highest Paying Jobs in Healthcare
Advanced practitioners are enjoying advanced wages, and two spots on a new top ten list of the highest paying jobs in healthcare.
The Public Is Clearly Confused about PAs and NPs
As the primary care physician shortage looms, and PAs and NPs are constantly called “the answer,” it seems patients are unaware of what they can even do.
Demand for Newly Certified PAs is Strong
Demand is high and the job market is strong for newly certified PAs, according to a new report by the National Commission of Certified Physician Assistants.