Pharmacy & Biological Sciences
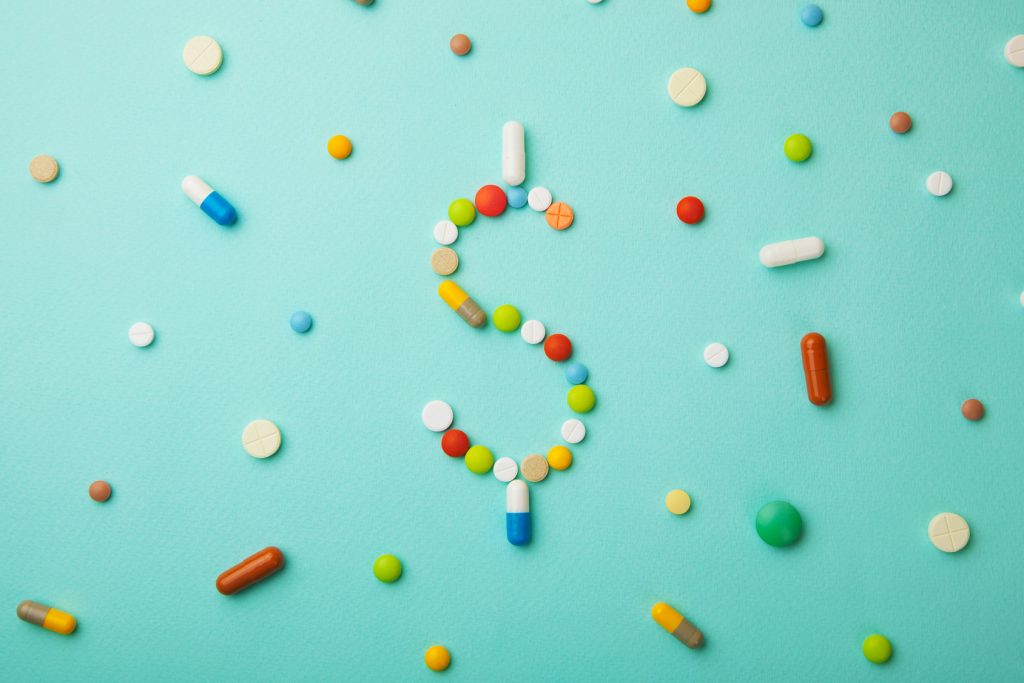
CategoryAmericans Rank Pharma Industry as Least Favorable
According to a new poll, even the U.S. federal government is more well-liked by Americans than the pharmaceutical industry.
Oklahoma’s ‘Precedent-Setting’ Suit Puts Opioid Drugmakers On Trial
All eyes were on Oklahoma last week, when the first case in a flood of litigation against opioid drug manufacturers began Tuesday.
Heart Drug Spotlights Troubling Trends In Drug Marketing
Headlines proclaimed a potential game changer in treating cardiovascular disease—Vascepa—and company shares quickly soared, but the study behind the claim remains a mystery.
New Opioid Approved by FDA, Mere Days After Trump Signs Opioid Bill
On October 24th, President Trump signed a package of bills designed to confront and combat the nation’s opioid epidemic. On November 2nd, the FDA approved Dsuvia.
Global Pricing Plan Added To Trump’s Attack On Drug Prices, But Doubts Persist
The proposal would have Medicare base what it pays for some expensive drugs on the average prices in other industrialized countries.
New Drug to Treat the Flu Approved by FDA
The new drug, Xofluza, is the first new antiviral flu treatment with a novel mechanism of action approved by the FDA in nearly 20 years.
Large Number of Influencers on the “Health Care 50” are in Biopharma
Of the fifty most influential people innovating healthcare named by Time Magazine, those with ties to biopharma make up a large percentage.
TV Ads Must Disclose Drug Prices, Trump Administration Says
The Trump administration proposed a new rule this week which demands drug makers disclose list prices for medications in their TV commercials.
Mysterious Polio-Like Illness Baffles Medical Experts
A spike in cases of children with a rare neurological disease that causes polio-like symptoms has health officials scrambling to understand the illness.
Pharma Sales Growth Tied to Price Hikes
Of the roughly $23.3 billion in sales growth seen by 45 top pharmaceutical products, $14.3 billion of that has been tied to price increases, not demand.