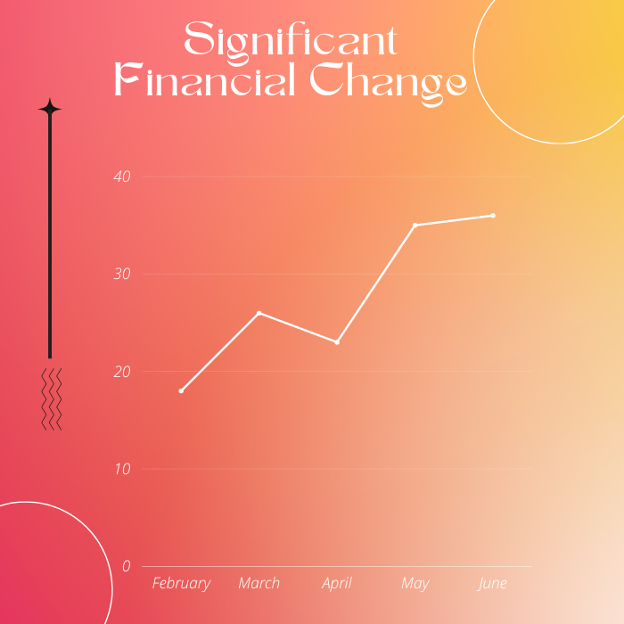
Turn Your Healthcare RCM Metrics into Action & Drive Significant Financial Change
Delivering standard medical aid to the patients while maintaining profitability is the primary objective of every health care provider. Achieving this balance is no doubt the key to a successful health care business. Moreover, physicians seem more interested in keeping their finances stabilized than ever before.
Achieving these financial goals are only possible through the effective management of the entire revenue cycle. Such as; patients’ scheduling, registration, charge entry, medical coding, claims submission, follow up, denial management, AR recovery and payment posting. However, we’ve been talking a lot about determining the key performance indicators to measure the effectiveness of the revenue cycle. No doubt, determining the RCM KPIs is the key to know where your business stands in terms of profitability & productivity. So, once you determine the key metrics, then what’s next?
Your financial success doesn’t just revolve around knowing the key performance indicators. But it’s all about taking steps to create and develop a strategic plan to accelerate your revenue cycle management. Turning the key RCM metrics into action can actually take your practice’s financial goals to another level. Do you want to create a strong financial plan but don’t know where to get started?
In this article, I have come up with proven strategies to help you in deploying a solid plan to take your health care business to the highest levels of profitability.
Know
First of all, decide the key performance indicators to track the performance of your physician billing system. KPIs can help medical care providers to increase the accuracy and the financial viability of their practice. However, the most common RCM metrics are as follow;
➔ Days in Accounts Receivable
➔ Clean claims ratio (CCR)
➔ Denial rate
➔ Bad debt rate
➔ Net collections ratio
➔ Gross collection rate
➔ Referral Rates
So, decide the key performance indicators, then figure out how to track them effectively, collect data and analyze it. No doubt doing so takes a lot of investment in terms of both, time as well as money. Successful execution of these tasks doesn’t mean you have done it yet. Your goal must be to collect 100 percent of net revenue. Just make it more comprehensive, for example, the data shows that your net collections are only at 90%. Which means that you are lagging behind your revenue goals. Now the next step is digging deeper into your medical billing systems to know the major causes. Which are holding you back from catching up with the billing collection targets. For instance, if you find that missing 5% revenue is due to the failure to collect the patient’s copays. And the remaining 5 percent is stuck in excessive claim denials due to certain reasons. It may seem like a small percentage. But it can cost millions of dollars in terms of lost revenue. The most common reasons behind insurance claims denials are:
➔ Insufficient or lack of documentation that supports medical necessity.
➔ Incorrect charge capture.
➔ Missing/ incorrect patients’ demographic as well as insurance information.
➔ Lack of prior authorization.
➔ Invalid medical codes.
➔ Duplicate billing.
Do you find the reasons behind revenue leakage? If so, then Good Job! Now you have a complete understanding of how much money you are losing & why you’re missing it. It will pave the way to take further action to improve your billing collections.
Plan
Now you get to know how many dollars you are leaving at the table. And performed the detailed root cause analysis to get to the major causes of the problem. Now it’s time to make a proper plan to eliminate those issues. For instance, if the above-mentioned factors are leading to the claim denials and eventually revenue loss. Then move ahead. Now get your entire revenue cycle team onboard including front desk and back-end teams to discuss what is going wrong and which action you can take to eliminate the red flags in the revenue cycle management.
Furthermore, make sure that each person in the chain understands his/her role and is working diligently to execute their tasks in an efficient manner. More importantly, physicians should make sure that the rules are being assigned to the staff according to their skills as well as capabilities. Along with the assistance of the revenue leaders and your RCM staff, develop a method to correct the problem. Let’s take another example. If the incorrect medical documentation or the manual process of data collection, processing and medical billing is the reason behind declined reimbursements.
Then invest in the staff training and more importantly automation of the entire urology medical billing _ from patients scheduling to payment posting and all in between. Along with planning to transition from manual to advanced billing technology, also pay attention to the training of the administrative staff. At this stage, health care professionals should set quantifiable goals. That may include the desired percentage of clean medical claims i.e., 99%, and a timeline to achieve it. The best thing you can do is convert your plan into a precise and accurate document.
Implement
With a plan and goals in place, it’s the right time to implement the plan that you’ve made so far. As we have earlier taken the example of manual billing methods and automation. So, you have decided to invest in automation. Make a budget for the purchase and maintenance of the cutting-edge practice management solutions i.e. EHR systems. Purchase the software and ensure its successful deployment within your physician practice.
After the implementation of the Electronic Health Records (EHR), the next step is staff training. Because the utilization of EHR isn’t beneficial until your administrative staff have a complete know-how of its effective use. Providers need to understand that embracing innovation isn’t easy for their staff. So, give them time to understand the things, set a positive tone and help your team understand their tasks.
Concluding Remarks
Know, plan and implement solutions according to your financial needs and areas that need improvements. Once you implement the plans you need to track results and continue to review data and analytics to make sure the plan is working. Compare the outcomes before and after the implementation. Remember! Don’t forget to celebrate victories and give credits to keep your team motivated as well as onboard.
Thus, this three-step approach can be applied to each key performance indicator you use to measure the success of your revenue cycle management. No doubt, it’s a daunting task. But you can simplify it by outsourcing your medical billing services to a professional billing collection agency. Outsourced RCM experts not only streamline your reimbursements. But also help you to determine, track and improve the key performance indicators, to ensure the continued financial stability as well as the sustainability of your practice.
I have a B.S in Human Services from Virginia Tech. I have worked in the medical billing and coding field for over 6 years. Currently, I am converting my passion into my words & writing content for publications regarding RCM.
Disclaimer: The viewpoint expressed in this article is the opinion of the author and is not necessarily the viewpoint of the owners or employees at Healthcare Staffing Innovations, LLC.
