Advanced Practice
CategoryRebranding of PA Title Moves Forward
The AAPA has announced they have selected a world-renowned branding firm to begin investigating rebranding the physician assistant title.
New App Connects Patients with Advanced Practitioners, RNs via Text
A new app is taking aim at the telehealth space–not to diagnose, but to triage–and advanced practitioners and RNs are the ones on call.
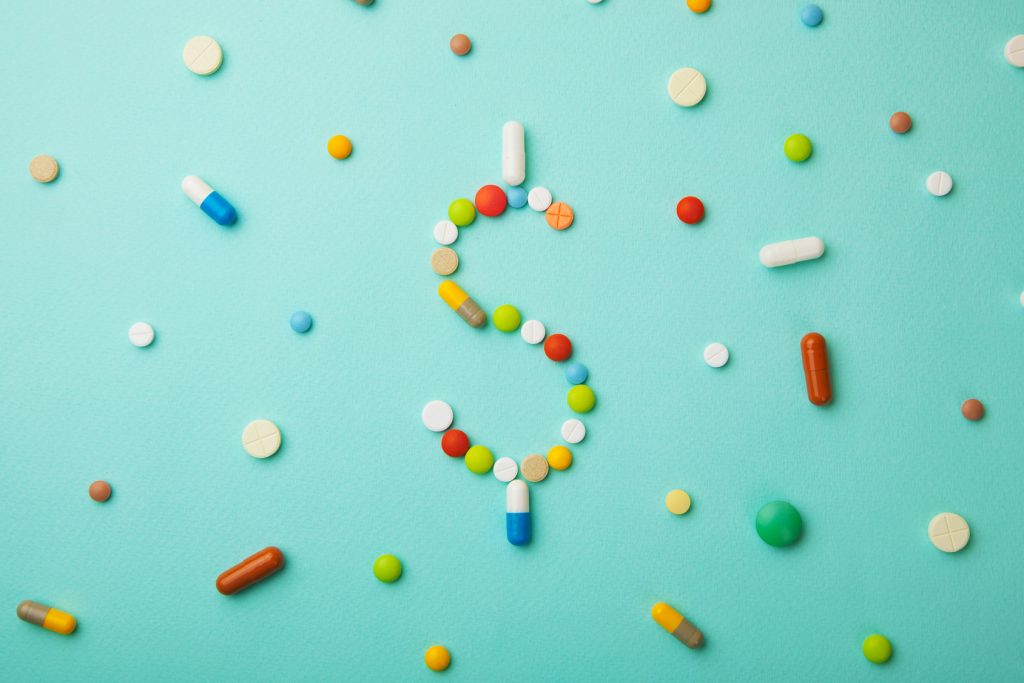
APRNs and PAs Ranked Among Highest Paying Jobs in Healthcare
Advanced practitioners are enjoying advanced wages, and two spots on a new top ten list of the highest paying jobs in healthcare.
Kim’s Blog: “See You Down The Road”
How do you ask patients about end-of-life wishes? Kimberly Spering, MSN, FNP-BC discusses her experience with having this crucial conversation.
The Public Is Clearly Confused about PAs and NPs
As the primary care physician shortage looms, and PAs and NPs are constantly called “the answer,” it seems patients are unaware of what they can even do.
Demand for Newly Certified PAs is Strong
Demand is high and the job market is strong for newly certified PAs, according to a new report by the National Commission of Certified Physician Assistants.
Kim’s Blog: What If The Priority of Our Visit is Addressing Social Needs and Non-Compliance
Kim Spering encourages you to look for the real reasons patients don’t show up on time, don’t take their medications, and seem to go against medical advice.
Entrepreneurship for Clinicians
Have you ever thought there might be more to your career than clinical practice? Explore the idea of entrepreneurship with Jordan Roberts and Dave Mittman.
Three Ways to Celebrate PA Week
Here are three ways to celebrate PAs, while also raising awareness of the profession’s significant impacts on healthcare, from October 6th through 12th.
Drama Series with NP Protagonist Heads to Netflix
A new romance drama series with a nurse practitioner at its heart is headed to the small screen, bringing exposure to the NP profession through entertainment.