Advanced Practice
CategoryHow Much PAs and NPs Make in Every State
How much do PAs and NPs make across the U.S.? We found out. How does your salary stack up against the average?
Hiring Spotlight: CoreMedical Group
In this Hiring Spotlight, learn more about CoreMedical Group and the thousands of openings they have available for nurses, therapy professionals, and physicians.
NP Role Expansion Bill Passes Pennsylvania Senate
Nurse Practitioners saw another victory in their quest for full practice authority on Wednesday in the Pennsylvania Senate.
Maine Law Allows PAs, NPs, Midwives to Perform Abortions
When the bill goes into effect next June, Maine will be the eighth state to permit advanced practitioners to provide abortion services.
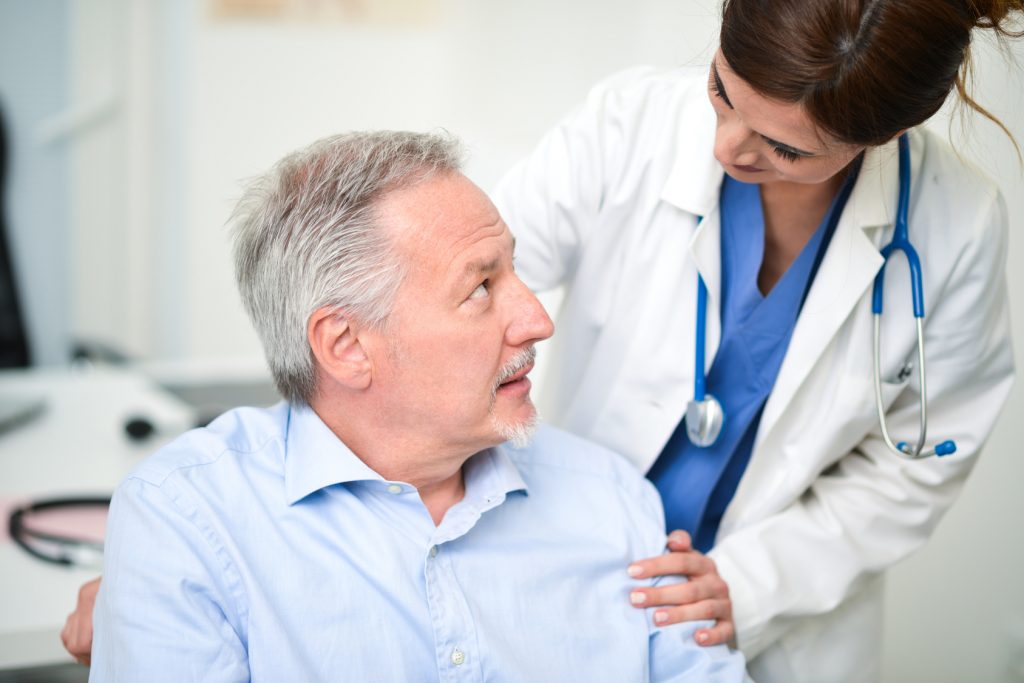
VA Study Supports Advanced Practitioner Led Care
A new study has found no clinically important differences in patient outcomes, regardless of whether their provider is a physician, PA, or NP.
Chipotle Offers Buy-One-Get-One Free Deal for Nurses
Free food alert! Chipotle locations across the U.S. and Canada will be offering a buy-one-get-one free deal for all nurses (including RNs, NPs, CNAs, and more) tomorrow, June 4th.
Critical Shortage of Pediatric NPs Looms
With the physician shortage in full swing and not enough PNPs joining the workforce, there is a growing hole in who will care for this nation’s children, with few answers in sight.
Barton Associates’ Locum Hero: Whitney Holmes, CNP
Earlier this year, Barton Associates announced the Locum Heroes campaign, with a focus on giving back to locum tenens providers who make a difference in their communities, near and far. In response, we received more than 100 nominations, each desc…
Fight to Expand Advanced Practitioner Roles Fails in Florida
House Bill 821 sought to grant autonomy to Advanced Practitioners in the state of Florida in an effort to expand access to care and affordability.
Report: PAs/NPs Provide Similar or Better Care than Doctors
A new report from a World Health Organization team indicates that non-physicians, such as PAs and NPs, provide comparable care to that of physicians.