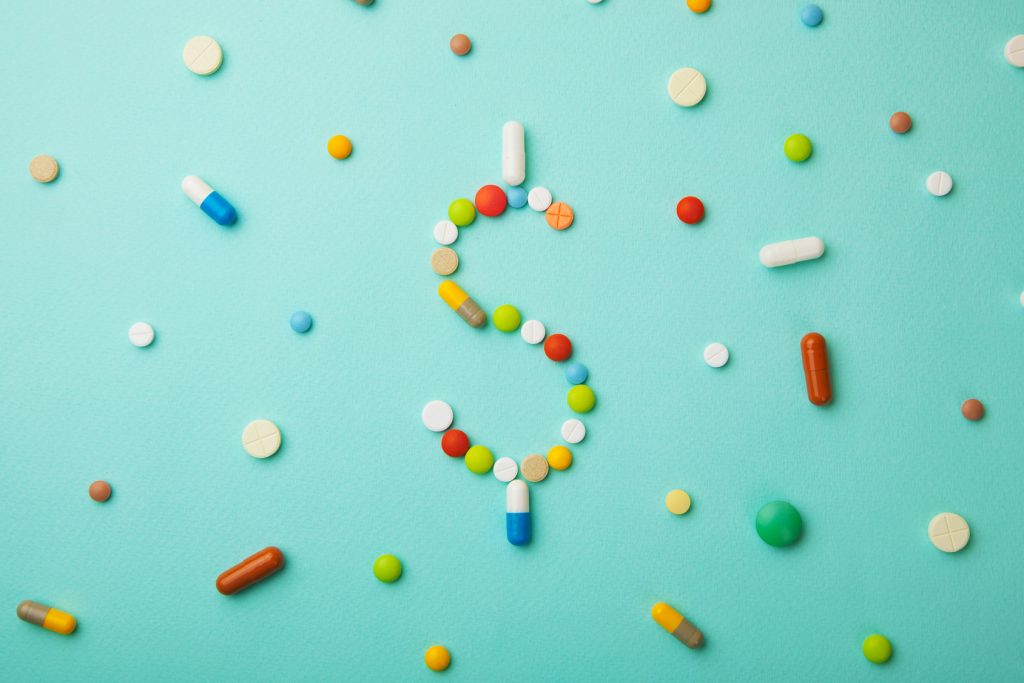
Landmark Decision Holds Drug Maker Responsible In Opioid Crisis
An estimated 130+ people die every day from opioid-related drug overdoses, and now a landmark decision in Oklahoma is holding one drug maker responsible.
Suicide Risk Among Nurses Higher than Non-Nurses
Nurses are at a higher risk of suicide than the general population according to the findings of the first national investigation into nurse suicide in over twenty years.
Superstar Athletes Popularize Unproven Stem Cell Procedures
Stem cell injections are costly, controversial, and unproven to be effective. So, why are professional athletes pushing them?
Physicians vs. Advanced Practitioners: Where Do You Stand?
A battle has been brewing between advanced practitioners seeking to expand their scope of practice and the physicians who oppose them. Where do you stand?
4 Technologies to Know About for Your Clinic
Keeping up with the latest technology is vital for the success of your clinic. Here are four to know about to help you innovate.
How Do You Deal with “I Want to See a Doctor”?
What do you do when a patient has the audacity to say, “I want to see a real doctor,” thus calling into question your qualifications?
Physicians and Suicidality: Identifying Risks and How to Help
Despite often being known as the healers, those who aim to save lives, it is estimated that as many as 400 physicians die by suicide in the U.S. each year.
4 Career Options That Don’t Require Traditional Medical Schooling
Healthcare offers many new jobs for individuals interested in a stable career, who don’t necessarily want to follow the traditional educational path.
The Highest Paying Job in Every State Is in Healthcare
Yes, you read that title correctly—the highest paying job in every single state in the United States is a healthcare job.
Americans Increasingly Sedentary, Not More Active
Americans are often portrayed as being lazy, and a new study finds that they are living up to that stereotype, getting more sedentary over time.