healthcare
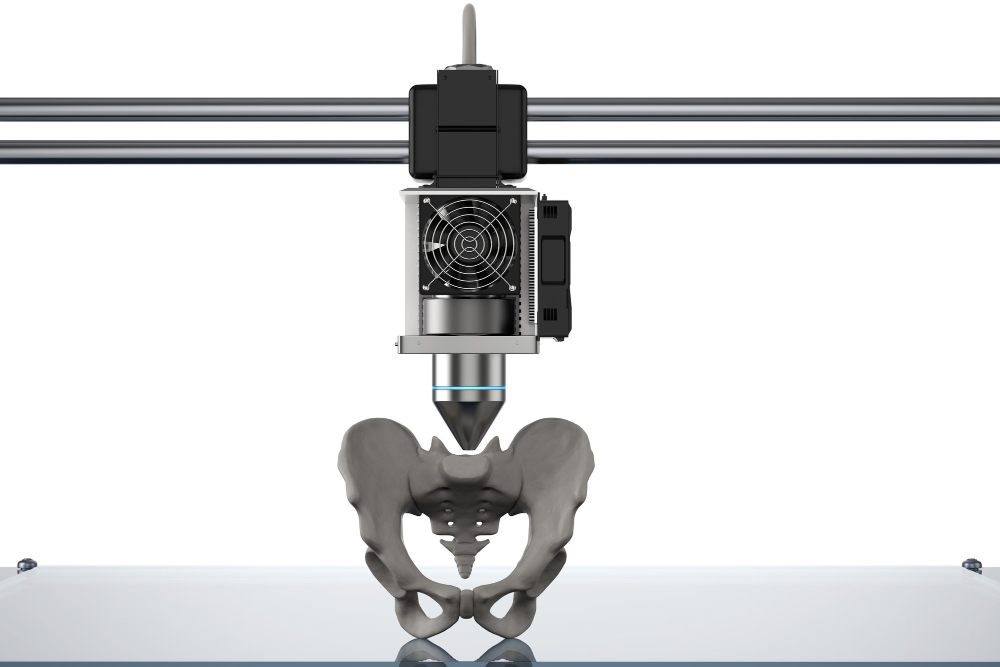
TagMedical 3D Printing Explained: From CT Scan to Custom Implants
Medical 3D printing has changed from a niche technology into a healthcare revolution. The global market is expected to reach $6.08 billion by 2027. Only three hospitals had in-house 3D printing facilities in 2010. This number jumped to 113 facilit…
Navigating the New Era of Patient-Centered Care in 2025
The year 2025 will mark a transformative period in healthcare as patient-centered care becomes increasingly prominent. This paradigm shift emphasizes treating patients as individuals with unique needs and preferences, fundamentally reshaping the p…
How Streamlining Hospital Processes Can Lead to Improved Patient Outcomes
We’ve all worked our way through the slow-moving bowels of the American healthcare system at one point or another. Maybe you had to fight your way to an appointment with a specialist who is apparently booked out six months in advance. Maybe you ne…
The Most In-Demand Specialties for NPs and PAs in 2024
As we near the end of 2024, the roles of Nurse Practitioners (NPs) and Physician Assistants (PAs) have become increasingly vital in the healthcare system. With a growing emphasis on accessible, high-quality patient care, these professionals are st…
How to Thrive in a Physician Shortage: Opportunities and Challenges
As we enter 2025, the healthcare industry is grappling with a significant challenge: a growing physician shortage. This shortage, driven by an aging population, increasing demand for healthcare services, and a wave of retirements among current phy…
How AI and Technology Are Transforming Nursing Practice
In 2024, the integration of Artificial Intelligence (AI) and advanced technologies into healthcare is not just a futuristic concept—it’s our present reality. Nurses, as frontline caregivers, are at the forefront of this technological revolution. L…
What Can Elderly Care Be Expected to Look Like in the Near Future?
At a certain point, humans who are lucky enough to make it to old age transition out of what we often call “preventative care.” Lifestyle adjustments that are designed to maintain their good health. People in the final stage of life develop chroni…
How Social Workers and Healthcare Providers Create Stronger Support Systems Together
Social workers are some of the most undervalued and overlooked professionals in today’s global economies. Despite a number of reasons to pursue social work, and that much of the social work accomplished is of great necessity and importance to huma…
The Rising Popularity of Home Healthcare and Its Impact on Nursing
Home healthcare is transforming the way patients receive medical care, rapidly gaining popularity as an alternative to traditional hospital or clinical settings. Driven by advancements in technology, a growing preference for personalized care, and…
How AI is Revolutionizing Treatment and Wellness
The Future of Healthcare
The health care industry is making some transformations, to turn over the industry in the hands of Artificial Intelligence (AI). The technology’s adoption in the health sector will focus on personalized care, with supervi…