physicians
TagNetworking in Healthcare: Strategies That Boost Careers and Improve Patient Care
Studies show that medical practitioners who build reliable networks get more referrals. This leads to a larger patient base and more profitable practice . Medical professionals know that our field runs on collaboration and knowledge sharing, espec…
The Physician Job Market Has Changed: Here’s What You Need to Know
The physician job market has changed by a lot in the last few years. A remarkable 62% of doctors have switched careers since 2022. This massive change shows a profession going through major upheaval, even with doctors and surgeons earning an attra…
New FDA-Approved Non-Opioid Pain Medicine: What Prescribers Need to Know
The FDA’s recent approval of Journavx (suzetrigine), a non-opioid pain medication, represents the most important breakthrough in pain management. Over 80 million Americans receive prescriptions for moderate-to-severe acute pain each year. This new…
The Rise of Functional Medicine: Root-Cause Healthcare for Chronic Conditions
The number of functional medicine (FM) practitioners in the U.S. has seen a dramatic rise, climbing from approximately 5,000 in 2010 to around 40,000 by 2020. Industry projections indicate continued growth in both employment opportunities and comp…
GLP-1 Thyroid Cancer Risk: What New Research Reveals for Physicians
New research shows that GLP-1 receptor agonists (GLP-1RAs) are linked to a increased risk of thyroid carcinomas. The hazard ratio stands at 1.58 (95% CI: 1.27-1.95) after 1-3 years of use. On top of that, these medications raise the risk of medull…
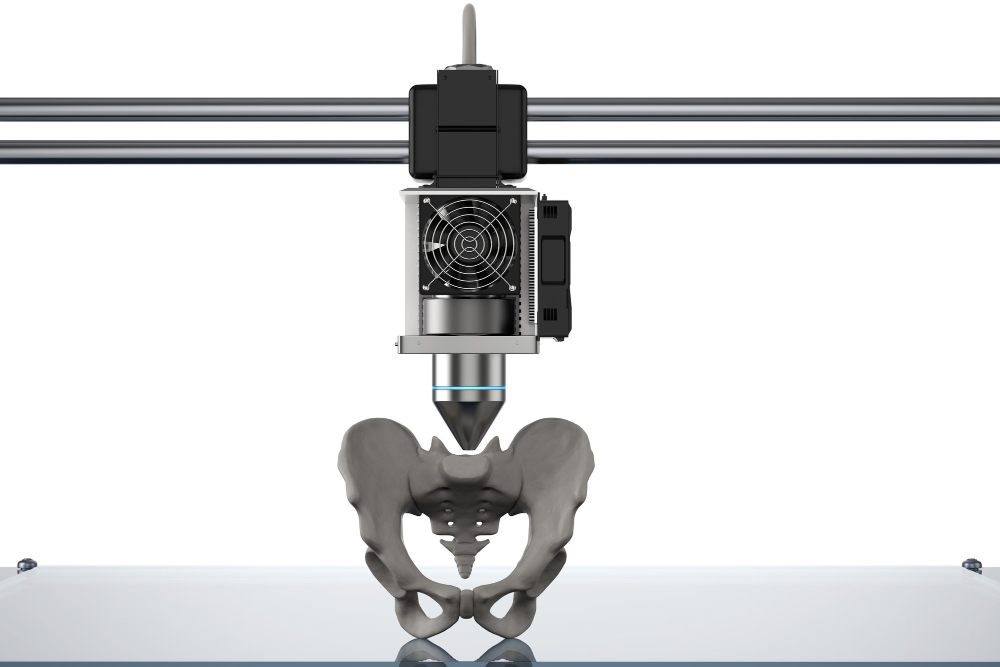
Medical 3D Printing Explained: From CT Scan to Custom Implants
Medical 3D printing has changed from a niche technology into a healthcare revolution. The global market is expected to reach $6.08 billion by 2027. Only three hospitals had in-house 3D printing facilities in 2010. This number jumped to 113 facilit…
Navigating the New Era of Patient-Centered Care in 2025
The year 2025 will mark a transformative period in healthcare as patient-centered care becomes increasingly prominent. This paradigm shift emphasizes treating patients as individuals with unique needs and preferences, fundamentally reshaping the p…
How Streamlining Hospital Processes Can Lead to Improved Patient Outcomes
We’ve all worked our way through the slow-moving bowels of the American healthcare system at one point or another. Maybe you had to fight your way to an appointment with a specialist who is apparently booked out six months in advance. Maybe you ne…
What Can Elderly Care Be Expected to Look Like in the Near Future?
At a certain point, humans who are lucky enough to make it to old age transition out of what we often call “preventative care.” Lifestyle adjustments that are designed to maintain their good health. People in the final stage of life develop chroni…
Seeking Second Opinions – Beneficial for Patients and Medical Teams
Maybe you’re the patient or on the medical team. Either way, referrals to a specialist are common, particularly when it becomes clear that the compliant patient isn’t improving despite following current clinical practice guidelines. At Skin, Bones…